Introduction to Revision Knee Replacement
To understand the revision of Knee Replacement, we must first be familiar as to what it refers to, Revision of knee replacement is the procedure used to restore or renew a failed first knee replacement. In the primary knee replacement, the implant or prosthesis that is made of metal or plastic components replaces the knee joint. There are many types of revision of knee replacement. Sometimes, only some components of the prosthesis have to be replaced and in other cases, the main three components of the knee – the femur, the tibia, and the patella, have to be replaced or repaired and with the help of augments, the bone has to be rebuilt or another procedure called bone grafting can also be performed.

Symptoms of Failed Knee Replacement
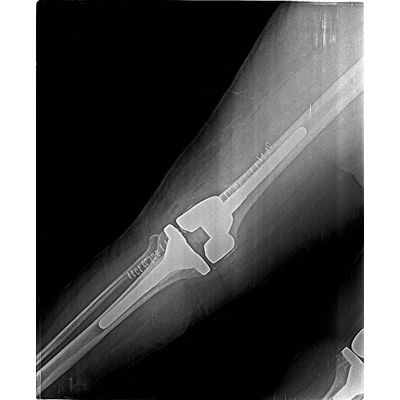
In most of the cases, the common symptom of the knee replacement failing is severe pain! and it turns out to be true in case of an infection or if the implant is loosening up. In addition to that, the other symptoms associated with the pain are swelling, redness around knee stiffness & sometimes instability of the joint or a limp caused due to the failure of the replaced joint. If the bone is damaged, then it becomes difficult for the doctor to use standard knee implants for revision of the knee replacement. In most of the cases, specialised implants that have longer and thicker stems are used so that they are deeper inside the bones for more support.


Indications for Revision Knee Replacement
With the revision of knee procedure being more complex than the original knee replacement, the operation would require additional planning and special equipment. When revision surgery is necessary, these are the symptoms that you will experience:
- Reduced stability or function of the knee
- Increased pain
- An infection (swelling, redness, leaking wounds, pus collection etc)
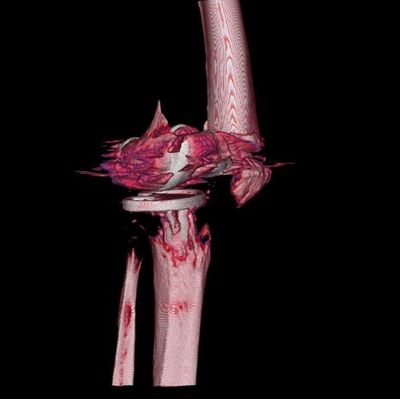
- A bone fracture
- An implant or device failure
In other cases, the prosthesis device might be wearing or breaking off by bits and pieces as tiny particles and accommodates around the knee.
The surgeon will help you determine the condition of your knee replacement and explains the functioning of the knee. Many tests are available which the surgeon carries out to determine the need for revision of primary knee replacement.
Infection
After several studies being done and post research analysis, it was found that the primary reason for a revision of a knee replacement was due to infection. 25% of the revision of knee replacement happens due to this reason. When artificially attached joints are infected, moving your knee becomes a difficult task and it is more painful compared to a loose joint. When there is infection in a replaced joint, it is a complication. To avoid further complications, we will have to replace the entire knee joint generally carried out in 2 stages. In the first operation, the artificial knee joint will be removed and that space will be filled with antibiotic laden cement spacer. This spacer will help you keep the tissues soft, and the antibiotic will reach out to this infected area. Depending on the patient, 6-12 weeks of antibiotic is provided to the patient. Once this procedure is completed, the second stage surgery is performed to implant a totally new set of implants.


Mechanical Loosening
As explained earlier, in most of the knee replacement a metal base will be attached to the tibia or the shin bone, upon which it has been secured by a plastic bearing and a metal cap that is then attached to the femur or the thigh bone. Surgeons usually prefer to use bone cement which is called as PMMA or Poly methyl methacrylate to make sure that the components hold themselves to the bone.
Even though these components are fixed right at the time of surgery, over a period of time they tend to become loose from the bone that has been supporting bone. When this happens, the patient will experience pain and difficulty in walking. This pain will get only worse with every passing day. Frequent X – Rays are suggested to make sure if the metal base is still attached to the femur.

Instability
One of the most troublesome parts of appropriately embedding a total knee is accomplishing the right balance of the delicate tissues around the knee. Prior to the surgery, if the knee test shows serious mal-alignment and weak and delicate tissues, the surgeon will have a tough battle on his hands to get the knee in balance. In the first operation if the tissues are not balanced right or if they become imbalanced with time, the joint tends to wear out prematurely which further leads to dislocation or subluxation of the knee joint. One of the other ways a knee can become unstable is when there is an injury. Here, if there is a serious injury, a surgical solution may be the only way to attain a satisfying stability. When the metal plates that are attached to the femur or the tibia, a fracture may disrupt the fixation to an extent where it might require a revision replacement. Once this complex fracture is stabilized, the revision of knee replacement will help stabilize and support the weight.


Preparation for Revision Knee Replacement
Every time a knee replacement surgery fails, it happens due to a different reasons and preparing for every knee replacement is unique. Blood tests CT scans and MRI tests are needed to evaluate the amount of bone loss in and around the current implant or around the rotational position of the prosthesis that is relative to the knee and the ankle. Despite careful preparation, there are greater risks involved when compared to the risks of primary knee replacement. The surgery is more complicated and consumes more time compared to the primary knee replacement. Hence it is advised that these surgeries are carried out by experienced surgeons only in this area of expertise. It is difficult to mobilize and protect soft tissues, blood vessels, and nerves and the prostheses are difficult to implement. It is important to note that the revised knee is never the same as the first knee replacement. The complications arising out of these surgeries may be more difficult to deal with compared to primary total knee replacement.
Post-Operative Re-habilitation
After the revision knee replacement procedure, you will undergo the same recovery process like the primary knee replacement. This may include the consumption of blood thinners to prevent clots, physiotherapy, and medication. Initially, you will need assistance with walking. You can use a walking support device like walker (zimmer frame), a crutch and you’ll be under the care of physiotherapists for more than three months.