Revision Hip Replacement
Introduction to Revision Hip Replacement
To understand the revision of hip Replacement, we must first be familiar as to what it refers to. Revision of hip replacement is the procedure used to restore or renew a failed first hip replacement. In the primary hip replacement, the implant or prosthesis that is made of metal or plastic components replaces the hip joint. There are many types of revision of hip replacement. Sometimes, only some components of the prosthesis have to be replaced and in other cases, all the main components have to be replaced or repaired and with the help of augments, the bone has to be rebuilt or another procedure called bone grafting may have to be performed.
Symptoms of Failed Hip Replacement Surgery
In most of the cases, the common symptom of the hip replacement failing is severe pain! Other symptoms like difficulty/inability to walk and bear weight and or instability may also be present along with pain & swelling. If the bone is damaged, then it becomes difficult for the doctor to use standard hip implants for revision of the hip replacement. In most of the cases, specialised implants that have longer, and thicker stems are used so that they are deeper inside the bones for more support.
Indications for Revision Hip Replacement Surgery
With the revision of hip procedure being more complex than the original hip replacement, the operation would require additional planning and special equipment. When revision surgery is necessary, these are the symptoms that you will experience:
- Reduced stability or function of the hip
- Increased pain
- Signs & symptoms of infection such as pain, swelling, redness etc.
- A bone fracture (Peri-prosthetic fracture)
- An implant or device failure
- Implant Wear and Loosening
- Recurrent Dislocation
In other cases, the prosthesis device might be wearing or breaking off bits and pieces as tiny particles and accumulate around the hip.
The Doctors will help patients understand the condition of replaced hip and will conduct many tests to diagnose the reason for failure of primary hip replacement. Once certain about the diagnosis will suggest the appropriate further steps for Revision Hip Replacement
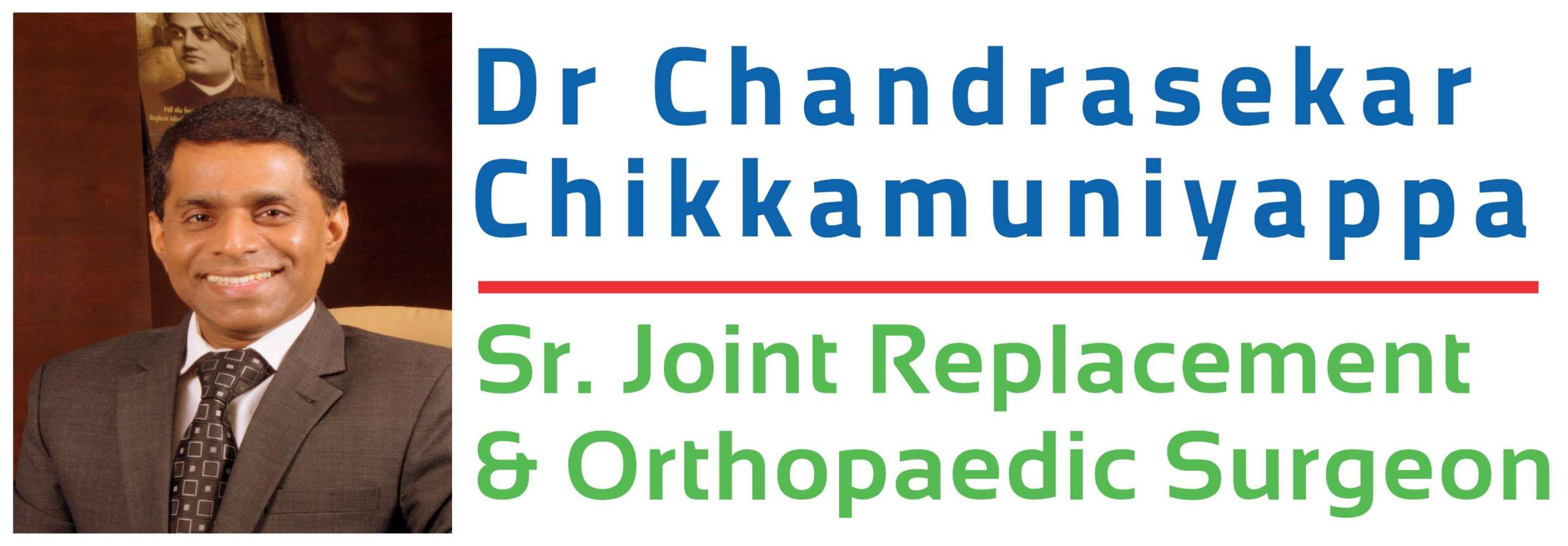
Infection
After several studies being done and post research analysis, it was found that the topmost reason for a revision of a hip replacement was due to infection. When bacteria attaches in and around the surface of the prosthesis (biofilm formation), the bone gets infected and infection can happen when you are in the hospital, when you go home, or after many years after the replacement. When artificially replaced joints are infected, moving your hip becomes a difficult task and it is more painful compared to a loose joint. When a total hip replaced joint is infected, it may begin to lose its attachment to the bone. To avoid further complications, we will have to replace the entire hip joint. The revision of hip replacement surgery can happen in many ways and to determine which procedure to use, the doctor will consider a lot of factors like:
- Determining the type of bacteria by doing culture and sensitivity (growing the bacteria in the lab and
- assessing their sensitivity to various antibiotics)
- Duration of the infection
- Severity of the infection
There are two types of surgeries performed for infected hip replacement surgery, they are:
- Debridement only:
- In this surgery, the surgeon will reopen the infected hip, wash or clear the bacteria present, and the ball and plastic liner is exchanged. Some implants are left inside after thorough cleansing. Post-surgery, the patient will be put on appropriate antibiotics that helps the patient in curing the infection.
- The second type of Surgery is Debridement & Implant Exchange. In this case, the existing set of implants are completely removed and after thorough debridement and cleansing exchanged for new set of implants. This exchange process can be done in two ways;
- Single stage Revision hip Replacement, In this scenario Debridement and implant exchange are done in the same sitting
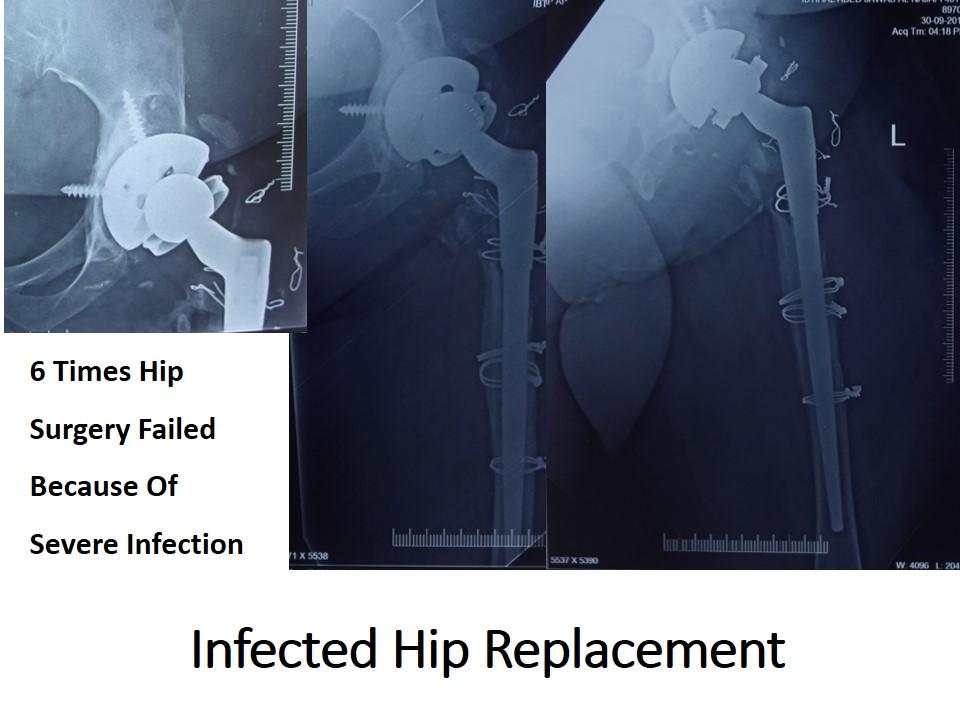
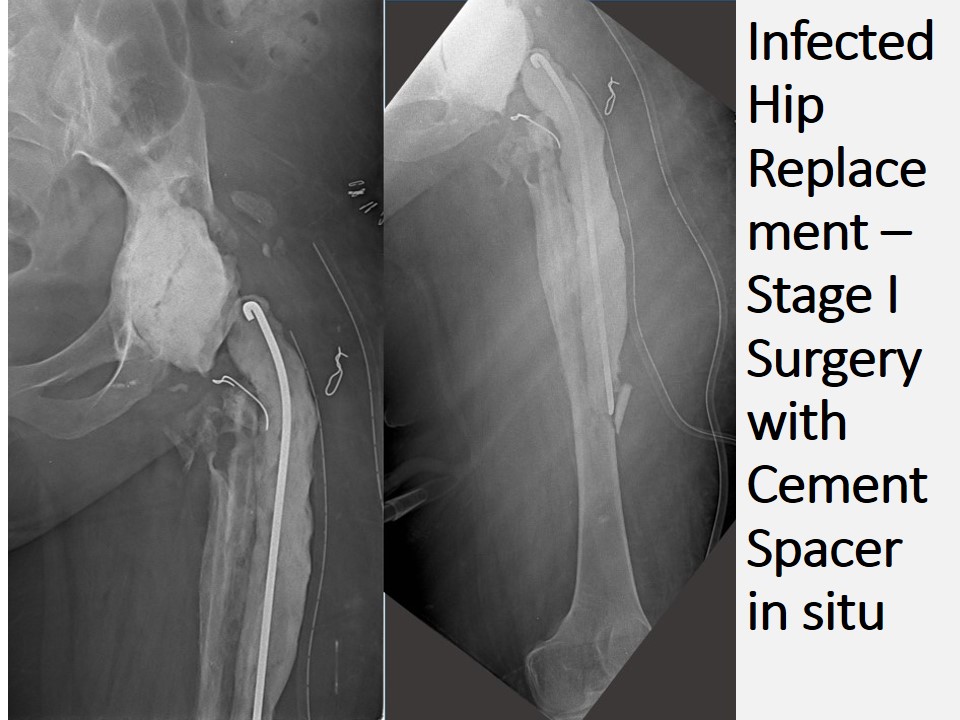
- Two stage Revision Hip Replacement, in this scenario in the first stage surgery Removal of all the existing implants, thorough debridement of the joint and Antibiotic loaded Cement spacer application is done. In the post-surgery period appropriate antibiotics are given and the patient is monitored for inflammatory markers like ESR (Erythrocyte Sedimentation Rate), CRP(C – reactive protein) and Total White cell counts etc. Once these inflammatory markers come under control the second stage surgery will be conducted in which removal of cement spacer and Revision Hip Replacement Surgery is conducted with a new set of Implants.
Mechanical Loosening
The hip replacement parts move against one another during regular activities of the patient. These movements are more in the physically active the patient, more the movement, and the faster is the wear. Repetitive movement & rubbing of the parts causes formation of small pieces of the wear particles. Plastic, cement, ceramic, or metal particles may be formed Depending on the type of hip replacement.
Our immune system recognizes all particles as foreign and generate an immune response. Reaction to these wear particles most of the times result in the destruction of bone this is termed as osteolysis. Once the bone destruction is severe enough, the implants of the replaced hip may become loose.
Apart from mechanical wear & tear leading to loosening of the prosthesis there are other forms of mechanical failure such as prosthesis breakage.
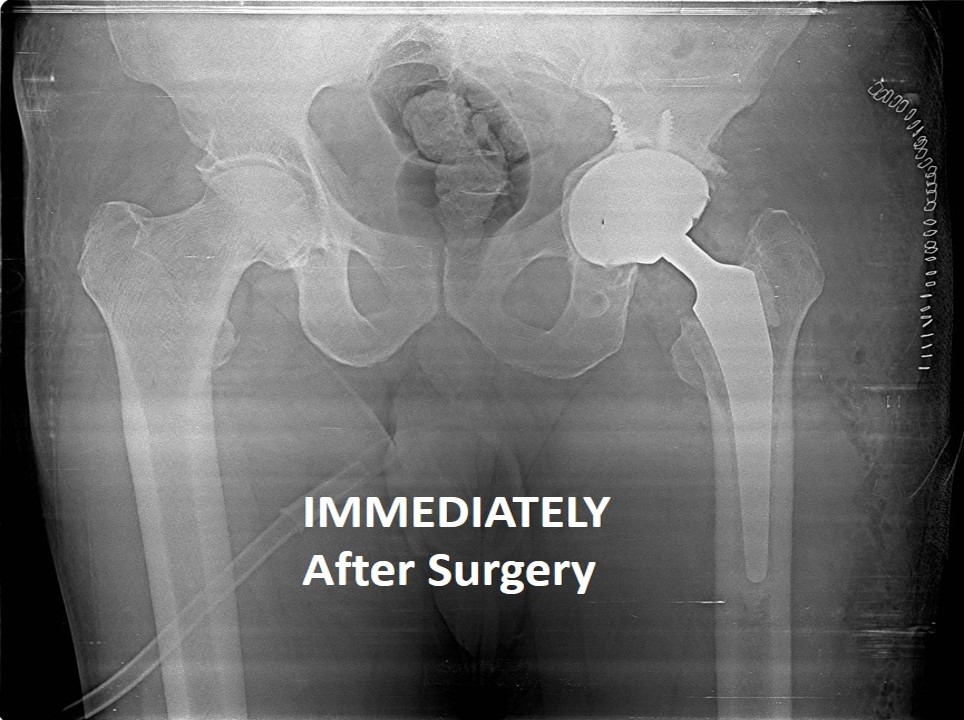
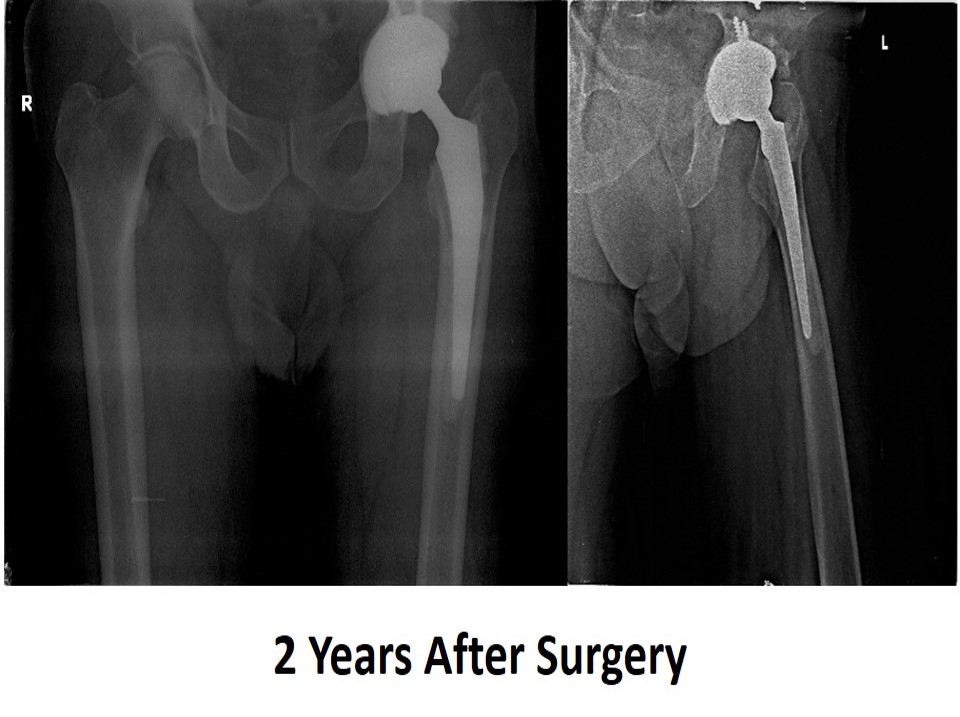
During Revision Hip Replacement all the worn out/loose/broken implants are removed and appropriate revision implants are used to reconstruct the new Hip.

Instability
Instability is one of the common reasons for revision hip replacement. Factors that contribute to instability after total hip replacement include Design of the implants used during the first time surgery, component position, technique and surgical approach used and also some of the patient related factors. Spinal mobility has also been considered as an important risk factor for dislocation after Hip replacement.
When Instability is determined as the cause for failure of Hip Replacement surgery, usually patient will undergo several tests including Radiographs, CT scans and/or MRI imaging and some blood tests, to determine the cause of instability. ‘Pseudotumours’ which may be present in some patients complicate the revision surgery situation.
Along with revising the implants and ensuring accurate component positioning, some of the other additional techniques used are using special implants like cups with ‘constrained liners’ or using tripolar/dual mobility implants. These measures usually ensure that the revised hip is most stable.
Preparation for Revision hip Replacement
Every time a hip replacement surgery fails, it happens due to a different reason and preparing for every revision hip replacement is unique. CT scans / MRI scans may be needed to evaluate the amount of bone loss in and around the current implant. These scans can also give information about the rotational position of the prosthesis that is relative to the hip knee and the ankle. Despite careful preparation, there are greater risks involved when compared to the risks of primary hip replacement. The surgery is more complicated and consumes more time compared to the primary hip replacement. It is difficult to mobilize and protect soft tissues, blood vessels, and nerves without causing any damage to them. It is important to note that the revised hip is never the same as the first hip replacement.
Outcomes of Revision hip Replacement
After the revision hip replacement procedure, you will undergo the similar recovery process like the primary hip replacement. This will include the consumption of blood thinners to prevent clots, physiotherapy, and medication. Initially, you will need assistance with walking. You can use a walking device like a walker (Zimmer frame), crutch or a cane. Physiotherapist will guide the recovery for as long as 3 months in the recovery period.